Harness the power of the Optum enterprise
Introducing new interventions in today's complex commercial market is risky. At Optum®, our programs and connections to all parts of the health care system allow you to test your new offerings in the real-world environment before expanding them to full scale.
Cross Optum programs turn evidence into action
In this fragmented health care landscape, life sciences organizations are faced with the challenge of how to connect the pieces. They’re asking how to:
- Improve efficiency of timely diagnosis
- Test new processes that could improve clinical decision-making and therapy adherence
- Discover effective ways to improve guidelines for directed therapy and evidence-based medicine
- Understand patient and provider behavior in the real world
- Educate patients on therapy options and the benefits of staying on track with their treatment
Small changes can make a big difference. The Cross Optum team works with life sciences companies and the larger UnitedHealth Group® enterprise to identify unmet needs, design and pilot engagement programs, and evaluate outcomes.

Connecting parts of the health care ecosystem
Our team uses implementation science to generate evidence that serves as a catalyst to improve the future of health care.

- Elevate the patient care experience
- Optimize patient treatment
- Reduce health care provider abrasion
- Improve health outcomes and costs
Key benefits
Clinical programs and process improvements to existing interactions help foster adoption across stakeholders. We focus on the following:
Disease awareness and prevention
Identify at-risk individuals and help resolve health care gaps.
Guideline-directed care
Improve quality and consistency of patient care across the health care ecosystem.
Treatment, intensification and adherence
Collaborate to increase adherence and improve outcomes.
Case study
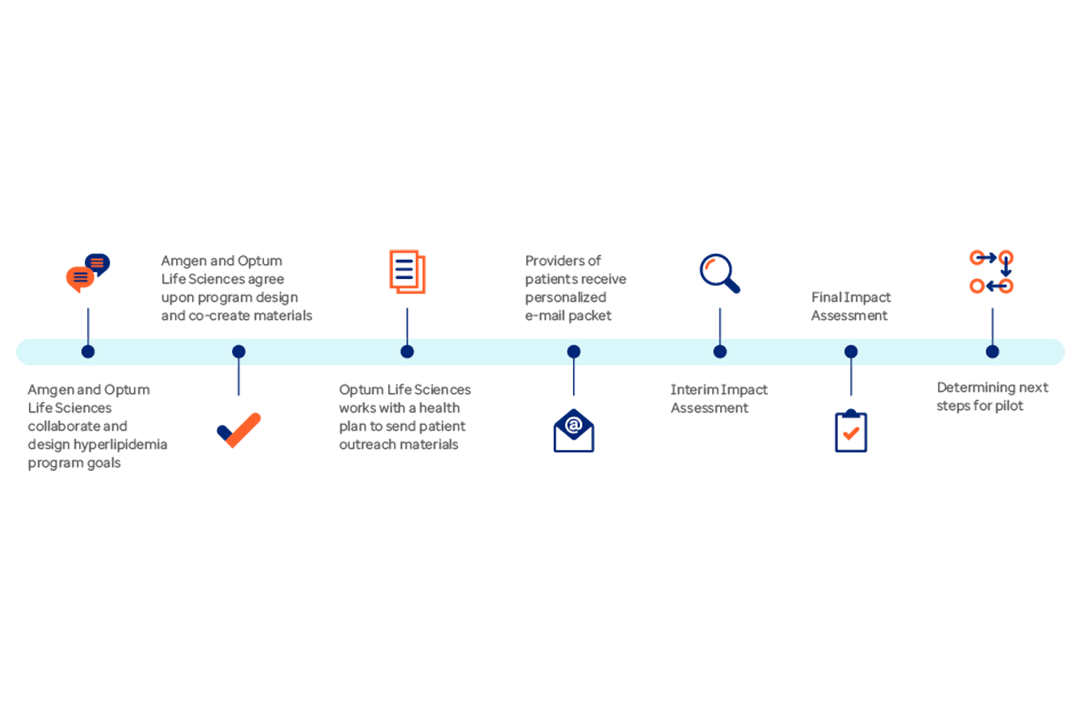
Lowering cardiovascular disease risk
An innovative program involving patient awareness and provider outreach helps improve patient use of lipid-lowering therapies.
Build evidence to reach and treat the right populations
Optum designed a program to introduce an assessment tool and prepare clinicians with training and a guide to aid diagnosis and treatment.
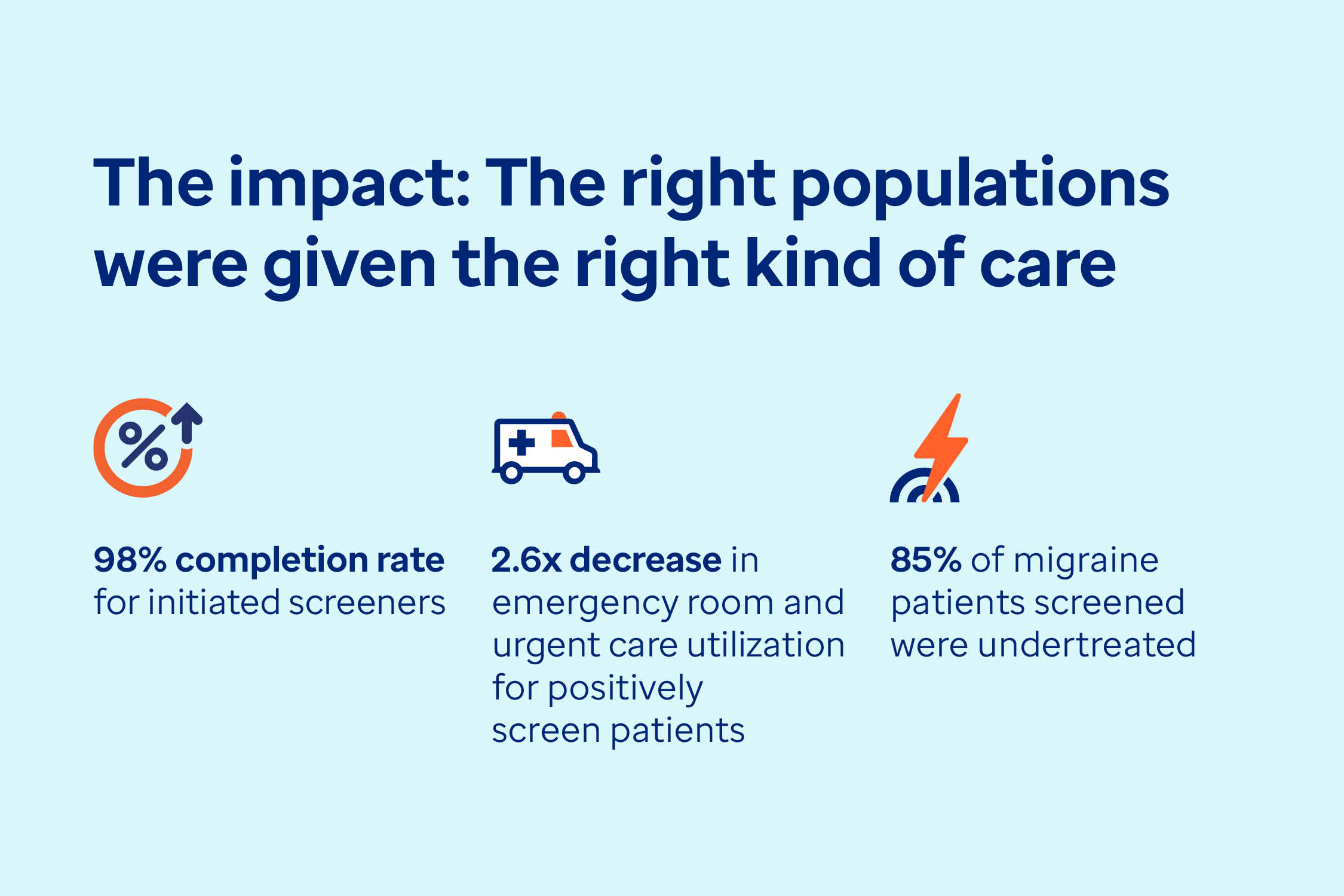
The impact: The right populations were given the right kind of care
- 98% completion rate for initiated screeners
- 2.6x decrease in ER and urgent care utilization for positively screened patients
- 85% of migraine patients screened were undertreated
Meet our experts
Olivia Banyon leads the Cross Optum Clinical Programs team with more than 20 years of experience in the life sciences, pharmaceutical and health care industries. Most recently, she was senior director of Innovative Solutions and Population Health at Sanofi. In this role, she led numerous pilot studies with large health systems, national and regional payers, and provider groups. Banyon has also worked for Pfizer and Merck-Medco, leading quality improvement and complex disease management programs nationally. She has built new companies from start-up to mature phases in clinical decision-making while mentoring and developing teams in the areas of adherence, disease management, predictive analytics, patient education, and wellness and behavioral change science. Banyon holds a Master of Public Health in Epidemiology from New York Medical College.
Tina Kelley focuses on program design and execution for the Cross Optum Clinical Programs team. She has worked in research and development roles across UnitedHealth Group for 12 years focusing on innovative solutions for the health care system, including telehealth, chronic care management and alternative care delivery models. As a senior leader with over 20 years of experience in retail, financial services, consulting and health care verticals, Kelley has established deep expertise for business enablement through the design and development of strategic programs that contribute to bottom-line growth. Her passion is delivering innovative engagements that contribute to advancing the health care industry. She holds a Bachelor of Arts in Organizational Communication from the University of Minnesota.
Aimee Coughlin is a senior consultant on the Cross Optum Clinical Programs team, with over 20 years of experience in the life sciences, pharmaceutical and health care industries. As part of the Optum Access and Value Strategy team, Coughlin led several types of consulting engagements, including real-world evidence needs and payer and provider engagement strategy. Most recently as part of the Cross Optum team, she has managed clinical programs in various therapeutic areas, including diabetes, cardiovascular disease, asthma and migraine. Prior to Optum, Coughlin worked at Charles River Laboratories as a product manager where she led a highly successful drug discovery business unit. In this role, she was responsible for the development and execution of marketing strategy, sales forecasting, pricing strategy and sales team development. She holds a Bachelor of Arts in Biochemistry from St. Anselm College and a Master in Business Administration from Northeastern University.
Katherine Ferro has been with UnitedHealth Group for over 5 years. She started with UnitedHealthcare in the Population Health Accountable Care Organization division as a clinical transformation consultant, and then moved to support the enterprise strategy for social determinants of health for UHC members as a program consultant. Ferro joined Cross Optum in June 2021 and currently serves as a senior consultant. Prior to joining UnitedHealth Group, her previous work focused on health care innovation and improvement across various organizations, including technology organizations, provider support and consulting organizations, managed care organizations and wellness organizations. She is passionate about improving the health care system and the lives of patients, members and consumers. Ferro received her Master of Health Services Administration from the University of Kansas Medical School, her Master of Business Administration from the University of Kansas, and her Bachelor of Arts from the University of Notre Dame.
Nick Payne is a program consultant on the Cross Optum Clinical Programs team with over 15 years of experience spanning the payer, provider and life science sectors. He presently leads 4 clinical programs, helping direct the design, scoping, build and rollout of live patient interventions seeking to impact and transform health care delivery. Previously, Payne consulted for several national payers and large provider systems, helping to lead and direct a range of digital product initiatives, pilot and test chronic condition and device solutions at a large scale, and develop and define cross-organization partnerships to drive insight into health care cost and quality. He also brings a background and interest in international health care policy and analysis, having worked on clinical improvement and complex disease management programs within the United Kingdom and European Union. Payne holds a Bachelor of Arts in Economics and Politics from University of York and a Master in Business Administration from Durham University.
Dr. Kizzy Steward-Judie earned her Doctor of Pharmacy from Howard University College of Pharmacy in 2003. She began her managed care experience with UnitedHealthcare Community & State Prior Authorization Services in July of 2011. In 2014, she transitioned to Optum Population Health Services where she served as a clinical leader and pharmacy subject matter expert for the Fully Insured Patient Centered Care Model. Medication affordability and optimization, opportunity gaps in treatment care, and the development and implementation of new pharmacy programs and services were key responsibility areas within this role. Prior to joining UnitedHealth Group, Dr. Steward-Judie served as chief pharmacist at the University of Houston Student Health Center, where she was instrumental in achieving full accreditation, which enabled the university to attain Tier 1 Status. An expansive career background including retail, hospital, outpatient and ambulatory care offers Dr. Steward-Judie a unique perspective of the evolving health care landscape. In this role, she is responsible for the development and execution of marketing strategy, sales forecasting, pricing strategy and sales team development. She holds a Bachelor of Arts in Biochemistry from St. Anselm College and a Master in Business Administration from Northeastern University.
Maggie Reyes-Leczinski is a senior consultant for the Cross Optum team with over 18 years in the health care industry. Her experience includes working with both commercial and publicly funded health plans like Medicaid, Medicare and Child Health Plan Plus, clinically integrated networks and life sciences organizations. Reyes-Leczinski started with UnitedHealth Group in 2018 as a senior consultant with the UnitedHealthcare Medicare Advantage division. In this role, she developed market business plans to improve Star Rating performance by focusing on cost, quality and the member experience. Prior to joining UnitedHealth Group, she worked for the Pediatric Care Network to develop and implement population health initiatives for value-based contracts. Reyes-Leczinski joined the Cross Optum team in 2021 and leverages her experience in managed care, population health, change management techniques, and both small and large health care organization transformation to succeed in value-based care. She holds a Bachelor of Arts in Political Science from the University of Colorado, Denver.
Sheriden Beard is a senior research analyst for the Cross Optum team. She has a Master in Public Health from New York University and a background in clinical research and quality improvement. Previously, she worked for the New York State Department of Health AIDS Institute on their quality team, and for New York University supporting clinical research sponsored by the National Institutes of Health. She has helped developed screening tools and quality improvement trainings for use in primary care settings, as well as published literature in areas such as exercise physiology and community-based participatory research. Beard leverages her experience to bring public health and health equity-focused ideas into all Cross Optum programs.



